The link between artificial sweetener and Crohn’s disease and how the former affects the latter was revealed in a new study by researchers in Case Western Reserve University School. In an experiment conducted with Splenda – the artificial sweetener- it was found that it could aggravate a patient’s gut inflammatory condition by promoting bad bacteria.
The experiment was conducted on mice over a period of six weeks and it revealed a lot of factors. Splenda or sucralose spells disaster for mice infected with Crohn’s disease by augmenting the intestinal inflammation. The rodents free from this disease weren’t affected at all by Splenda intake. Scientists are, therefore, considering this aggravation as one of the side effects of artificial sweeteners.
How are the artificial sweetener and Crohn’s disease related?

Artificial sweeteners and Crohn’s disease has a linear relationship. Crohn’s disease causes inflammation of your digestive tract and intake of Splenda is just like adding fuel to fire. Symptoms in bowel disease due to artificial sweeteners could be extremely painful- reflected by severe diarrhea, blood in stool, tiredness, intense abdominal pain and rapid reduction in body weight.
There had been cases of feedback from around 15% of Crohn’s disease patients that intake of Splenda has exacerbated their conditions leading to intense pain.
Increase in Proteobacteria worsens the symptoms:
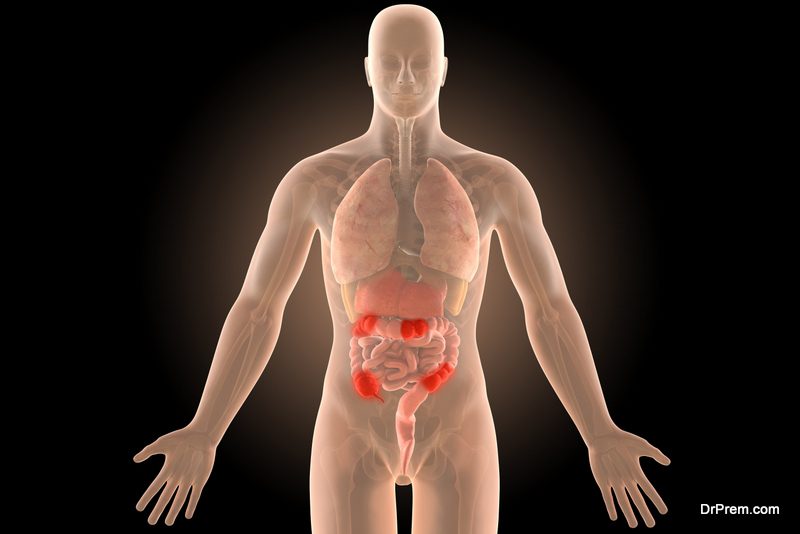
The recent discovery published in Inflammatory Bowel Diseases throws some light on actually what happens when mice with Crohn’s disease are fed with the artificial sweetener Splenda. It causes a spike in the number of Proteobacteria, which is a large phylum of microbes.
In fact, Proteobacteria is already known to contribute to various intestinal-tract related ailments in different species – including human beings. It is the outer membrane of Proteobacteria composed of lipopolysaccharides that trigger a strong immune response in the form of inflammation when it enters the human or animal body.
Around 50% of the mice under study were drawn from a bloodline suffering from Crohn’s disease. Rest of the population was from absolutely healthy stock. All were fed with water supplemented by Splenda. Side effects of artificial sweeteners on mice population came under intense study.
Splenda resulted in the excessive production of E. Coli in the intestine of mice and triggered bacterial puncturing through the intestinal lining. Those infected with Crohn’s disease were the sufferers, but the healthy group did perfectly well even with Splenda fed to them.
Normally, a certain number of Proteobacteria which includes E. Coli, salmonella, and legionellales are not harmful to the body; but when there is an excessive proliferation, health issues result. Symptoms in bowel disease due to artificial sweeteners have been well documented in a number of interviews with the suffering patients.
Artificial sweeteners trigger Myeloperoxidase activity:

The link between artificial sweeteners and Crohn’s disease is further established by a biochemical activity in the gut microbial population. Our white blood cells (leukocytes) contain an enzyme called Myeloperoxidase, which wipes out a number of microorganisms. Excessive availability of E. Coli in the gut triggers Myeloperoxidase activity in the bowel as the system tries to combat the intruder.
Inference of the experiment points out that intake of Splenda may enhance Myeloperoxidase synthesis in individuals having a history of Crohn’s disease, and inflammation in bowels is the eventual consequence.
In the study of metagenomic shotgun DNA sequencing, it was found that Splenda enhances proliferation of gut Proteobacteria, dysbiosis, as well as E.Coli and promotes biochemical MPO (myeloperoxidase) reactivity.
Though Splenda may cause microbiome alterations in both Crohn’s Disease prone mice and healthy mice, it did not cause any increased MPO activity in the healthy group. Consuming sucralose/maltodextrin loaded foods may aggravate the MPO intestinal activity only in those predisposed to inflammatory bowel disorder like Crohn’s disease.
Someday, these findings might make it possible to consider Proteobacteria and myeloperoxidase activity as fecal biomarkers to monitor the gut function and adjust the diets of the patients accordingly.
Patients with an inflammatory disease may need to avoid artificial sweeteners:

Splenda, which is 600 times as sweet as sugar, was introduced to the market back in 1998. It had reached the height of demand owing to its being similar in composition with other 4 approved and popular artificial sweeteners flooding the market.
With the recent findings confirming the relation between artificial sweetener and Crohn’s disease, patients suffering from this disease or other inflammatory bowel symptoms need to give a second thought regarding consuming artificial sweeteners.
Researchers of the above study also caution about the usage of other food additives like diet emulsifiers, which have also been observed to alter the gut microbiota in mice and promote colitis. There may be similar other scenarios which can put patients of Crohn’s disease at a higher risk of bowel inflammation.




