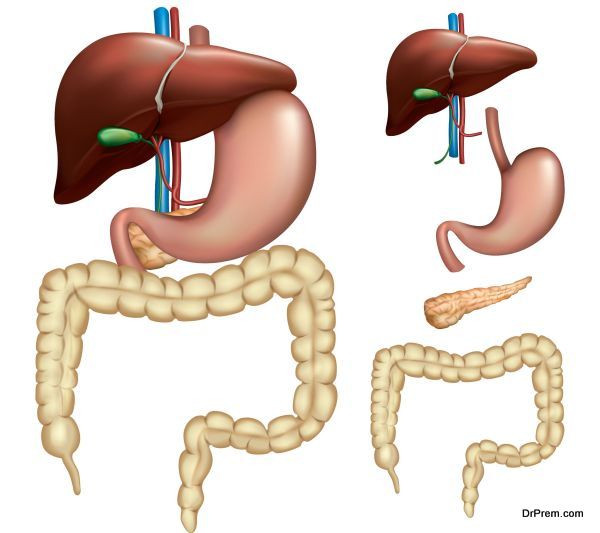
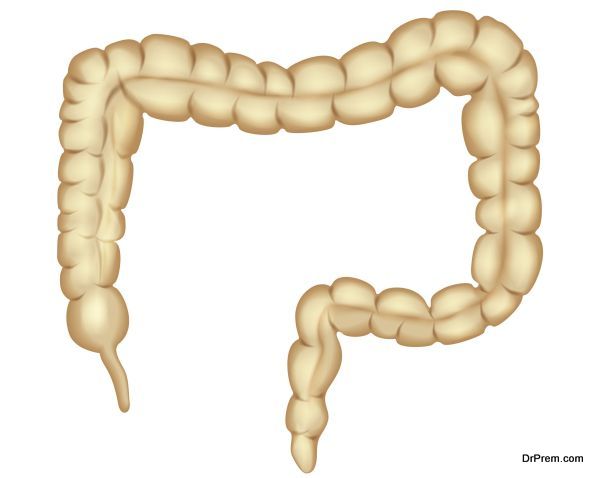
A cancerous growth in the colon or rectum, which is the large intestine of our body is known as colorectal cancer. The large intestine comprising of colon and rectum is the last part of our alimentary canal. Food passes from stomach and the small intestine through different phases of digestion and reaches the large intestine or colon where the absorption of water and minerals occur finally defecating the waste as stool through the rectum. Colorectal cancer that grows mostly from polyps is the third most common form of cancer in US.
Causes
Cancer in colon is not contagious but certain factors cause the spread of this disease some of which can be summarized as follows:
- Diet
Research studies have revealed that obese people consuming high fat content foods on a regular basis are predisposed to colorectal cancer. A high fat diet releases more cancer causing chemicals in the colon while high fiber diet rich in fruits, grains and nuts produce cancer fighting chemicals beneficial for the colon.
- Growth of colon polyps
Occurrence of colon polyps enhances the risk of cholorectal cancer. Benign polyps or adenomatous polyps appearing in colon should be removed timely to prevent the cancer. Initially, these polyps remain benign, but later due to chromosomal changes start spreading as cancerous cells.
- Ulcerative colitis
Prolonged inflammation of the inner lining of the colon due to ulcerative colitis often contributes to colorectal cancer. The risk is very high with chronic patients suffering for more than 8-10 years where the chances of developing precancerous cells are high. Ulcerative colitis patients with a family history of colon cancer are naturally at a very high risk.
- Genetic makeup
Though hereditary plays a role in developing colorectal cancer, it is surprising to note that 80% of colorectal cancer patients have no previous family incidence of this disease. Chromosomal damage changes the genetic makeup which gives rise to sporadic colon polyps gradually turning into cancerous form. Those inheriting the genes of colon cancer have a high chance of developing colon polyps giving rise to colorectal cancer at an early age.
- Familial Adenomatous polyposis (FAP)
It is a genetically inherited syndrome arising from the mutation of APC gene where the affected persons grow countless (hundreds or thousands) colon polyps in their early teens. If left undetected, these are likely to develop into colorectal cancer in the early 40s.
- Attenuated familial adenomatous polyposis (AFAP)
In this case, the person develops less than 100 colon polyps but is still at the high risk zone of developing colon cancer at a young age.
- Hereditary nonpolyposis colon cancer (Lynch Syndrome or HNPCC)
Another form of heredity related colon cancer where the person develops high cancer risk colon polyps in the right colon in early 30s or 40s. These persons also carry a high risk of developing cancer in the stomach, ovary and uterus.
- MYH Polyposis Syndrome
Another heredity linked syndrome arising due to abnormal genetic constitution where the person develops 10-100 colon polyps that turn into colon cancer at a very early age.
Symptoms
Symptoms of colon cancer can be summarized as follows:
- Frequent toilet visits
- Feeling that bowels are not clear after defecation
- Diarrhea and constipation
- Presence of blood in stools
- Pain and bloating of abdomen
- Feeling exhausted
- Unexplained weight loss
- Detection of lump in tummy or back passage
- Severe iron deficiency
The symptoms may be caused due to other ailments and should be confirmed only by medical practitioner.
Diagnosis and Treatment
The initial diagnosis starts with the following screening tests to detect precancerous or early stage and prevent the spread of the disease.
- Colonoscopy is performed to detect abnormal growths in colon.
- Blood tests are done to determine the presence of carcinogenic chemical CEA
- Removal of colon polyps and proper treatment of precancerous conditions
Treatment
After the confirmation of colorectal cancer comes the staging of the condition to carry out a guided treatment. The staging is confirmed through CT scans and X-Rays.
Stage 0 – Cancer detected at the innermost lining of the colon. Surgery is done to remove the tumor or cancerous areas. Highest survival chance of the patient.
Stage I – Cancer spread beyond the inner second and third layers of colon but not permeated the outermost wall. Aggressive surgery is required to remove the affected tissue. Has high potential of cure.
Stage II – Affects larger areas crossing the muscular colon wall but the surrounding lymph nodes remain unaffected. Surgical removal of a larger area is done often followed by chemotherapy.
Stage III – The cancer spreads to more than one or two lymph nodes or even more than that. Surgery is required to remove the affected areas including all the lymph nodes followed by chemotherapy. Radiation therapy may be suggested in case of larger tumors affecting other areas of the colon.
Stage IV – The cancer attacks other vital organs such as liver and lungs. The lymph nodes may or may not be affected. Removal of the entire affected area including the surrounding tissues through aggressive surgery is done followed by higher doses of chemotherapy. Radiation therapy is administered to relieve pain and discomfort.
Colorectal cancer can be detected through regular screening and the survival rate from this ailment is appreciably high provided proper treatments are administered timely.